The United States Cost of Dementia Project provides comprehensive, national, annual estimates of the total cost of dementia and builds the capacity of researchers and policymakers to address the economic consequences of dementia.
Why estimate the cost of dementia?
The economic impact of dementia in the U.S. is rising as the population ages. The impact goes beyond medical costs and includes hours of unpaid care by family and friends, earnings losses, and declines in quality of life affecting the lives of persons living with dementia and their families.
Understanding who bears what costs and when is key to decision making about resource allocation and priorities. As prevention, treatment, and policies change, these costs will evolve. By measuring the trends over time, we can better inform evidence-based strategies to lessen the financial impact of dementia for everyone.
How many people in the U.S. are living with dementia?
In 2025, there are 5.6 million people living with dementia in the United States, with 5.0 million ages 65 and older. Dementia refers to a group of symptoms, including memory loss, difficulty with language, problem-solving, and other thinking abilities, that are severe enough to disrupt daily life. Alzheimer’s disease is the most common cause of dementia.
What is the annual cost of dementia in the U.S.?
Total cost of dementia is $781 billion (2025 dollars).
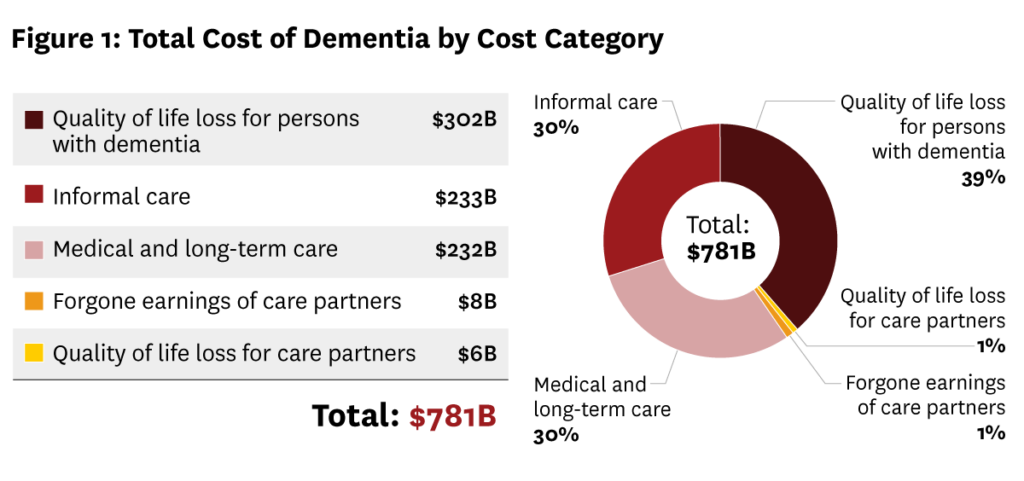
The medical and long-term care costs for dementia total $232 billion. Families and friends provide 6.8 billion hours of care, which is worth $233 billion.1 Many care partners also cut back on work or leave their jobs, leading to a loss of $8 billion in annual earnings.2 In addition to economic loss, people with dementia and their care partners experience a significant loss in quality of life, valued at $302 billion for those living with dementia and $6 billion for their care partners.3
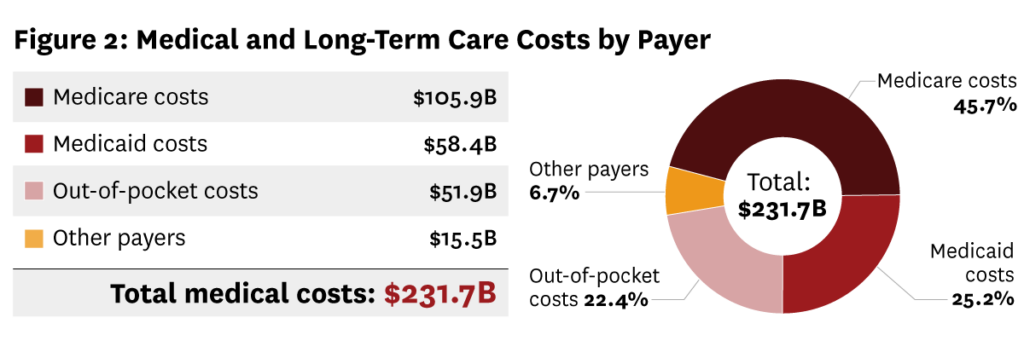
Among the $232 billion in medical and long-term care costs, $106 billion are borne by Medicare, $58 billion by Medicaid, $52 billion is out-of-pocket spending for individuals and families, and $16 billion is borne other payers, such as private health insurance.
How do we measure the costs?
We built the United States Cost of Dementia Model (USCDM) to estimate annual costs of dementia. It is a dynamic microsimulation model that uses data from individuals on their health and health care costs, work status, family and caregiving arrangement and personal finances, and how these change over time, to measure costs of dementia today and in the future. By using this approach, we can better understand how dementia impacts the lives of persons living with dementia and their families and care partners. USCDM uses nationally representative data from sources such as the Health and Retirement Study (HRS) and the Centers for Medicare and Medicaid Services to provide accurate estimates for the entire U.S. population. The project will seek to uncover all types of costs to provide the most comprehensive estimate of the national cost of dementia to date. (Learn more about how we measure the costs here.)
How can our model help reduce the consequences of dementia?
The model is a flexible tool that allows researchers and policymakers to explore how changes in prevention, diagnostics, and treatments affect costs for patients, payers and society. It can be used to analyze how health care policies or changes in the caregiving workforce influence dementia cost trends. With this information, key stakeholders can better evaluate the value of interventions and the ways in which policies and regulations may impact costs in order to address drivers of costs.
Who is involved in the project?
Leadership:
Julie Zissimopoulos, PhD
Co-Director, Aging and Cognition Program,
USC Schaeffer Center for Health Policy & Economics
Professor, USC Price School of Public Policy
Dana Goldman, PhD
Founding Director,
USC Schaeffer Institute for Public Policy & Government Service
University Professor of Public Policy, Pharmacy & Economics
The Team:
Led by Julie Zissimopoulos and Dana Goldman, the team includes researchers from the USC Schaeffer Center for Health Policy & Economics, the USC Price School of Public Policy, the Mann School of Pharmacy and Pharmaceutical Sciences, the Davis School of Gerontology, the Viterbi School of Engineering, the Alzheimer’s Association, and the University of Pennsylvania. Researchers from other institutions provide additional guidance. The multidisciplinary team includes experts in clinical care, neuroscience, gerontology, policy, economics, engineering, and drug development. To ensure the model is practical, the project regularly consults with persons living with dementia, their care partners, and experts in public health and dementia care. Any errors or omissions are the sole responsibility of the project team.
The U.S. Cost of Dementia Project is funded by a cooperative agreement with the National Institute on Aging, part of the National Institutes of Health (#U01AG086827).
A press release about this report is available here.
- Hours valued at a replacement rate of $34.5/hour. Hours valued using opportunity cost is $247 billion.
- Earnings loss is calculated by estimating annual earnings of middle aged adults who have parents with dementia and comparing this to a scenario where the parents of these adults do not have dementia assuming labor force participation rates equal to similar adults with parents without dementia.
- We estimate the Quality-Adjusted Life Years (QALYs) of individuals with dementia which considers various aspects of health, like cognition and function. We estimate this again assuming people with dementia had mild cognitive impairment instead and did not progress to dementia. We compare the difference in QALYs and value the difference in QALYs at $150,000 per QALY. We assume a differential of 0.01 QALYs between care partners and persons who do not provide care.




