Antibiotics prescribed inappropriately waste resources, can cause health complications and have helped give rise to antibiotic-resistant “superbugs,” while the opioid crisis claims more than 115 lives every day.
Schaeffer Center researchers Jason Doctor and Daniella Meeker have employed theories of behavioral economics — or nudges — to influence provider prescribing behavior without reducing their autonomy. Their research has proved so effective in reducing unnecessary prescriptions that the Centers for Disease Control and Prevention has lauded one strategy — posted pledges — as a “best practice.”
A growing number of public health departments in the U.S. as well as the United Kingdom have reached out to Doctor to better understand nudges and how to implement the interventions he has developed. In recent years, Doctor has leveraged these insights in new research targeted at opioid prescribing. “Our studies suggest that simple and inexpensive tactics, grounded in scientific insights about human behavior, can be extremely effective in addressing public health problems,” Doctor says.
Opioid Reduction
Published in Science, a study conducted by Doctor highlighted an important gap in the care system: Many clinicians never learn of the deaths of patients from opioid overdose, as they simply disappear from their practice. The nudge was simple — the researchers randomly selected half the study participants to receive a notification from the county medical examiner when a patient to whom they had prescribed opioids suffered a fatal overdose.
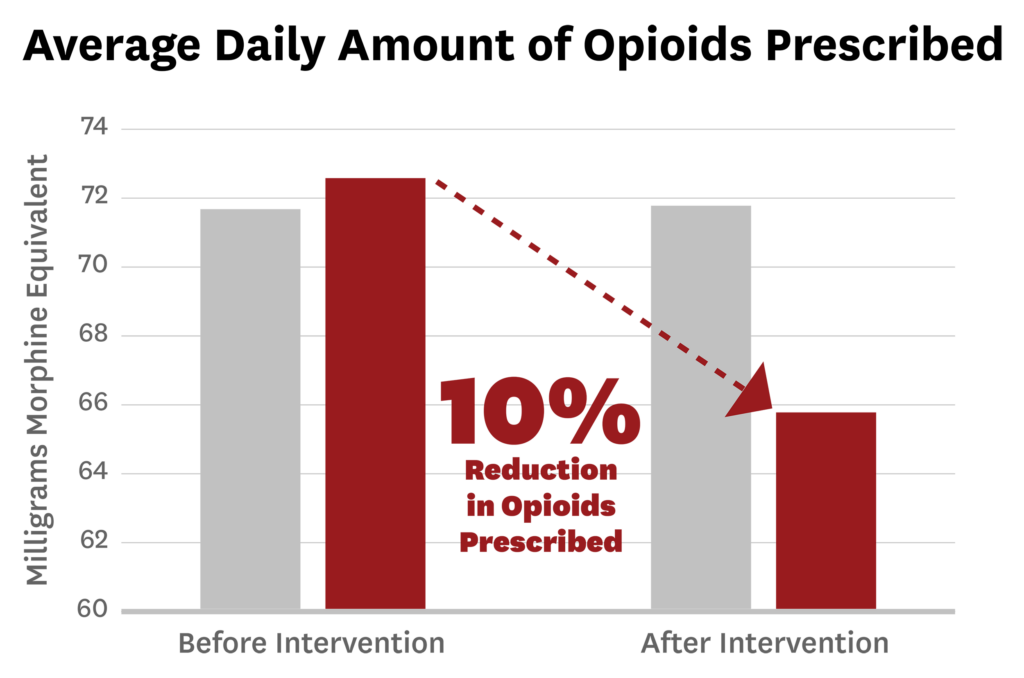
In the three months after they received the letter, the clinicians’ opioid prescribing decreased by nearly 10 percent compared to the group not receiving a letter. In addition, they were 7 percent less likely to start a new patient on opioids and less likely to prescribe higher doses.
Following the publication of the study in Science, multiple local and state agencies reached out to Doctor for guidance on implementation, including the L.A. County Board of Supervisors, which voted unanimously in favor of a feasibility study on how to implement such an intervention in Los Angeles. The results are particularly exciting given that more traditional state regulations involving mandated limits on opioids have not had much impact.
The authors point to the simplicity of the new approach, which provides an important missing piece of clinical information to physicians. This intervention is easily scalable nationwide as existing state and national resources already track overdose deaths associated with prescription and illicit drugs. For more, see the infographic about the study here.
Novel Nudges
Before opioids, Doctor led studies aimed at identifying solutions for unnecessary antibiotics prescriptions. He and colleagues, including Meeker and Tara Knight, analyzed the effects of easily adopted “nudges” to reduce over-prescribing, including:
- Posted pledges — having physicians hang posters in their examination rooms that explain safe antibiotic use and that include a signed promise to adhere to proper prescription guidelines
- Accountable justification — programming a prompt to appear when physicians update a patient’s electronic chart that asks them to justify any antibiotic prescriptions for acute respiratory infections
- Peer comparison — periodically emailing participating physicians with their inappropriate antibiotic prescription rates compared to those of top-performing doctors
Schaeffer Center Impact
Following publication of the Schaeffer study on posted pledges, the Centers for Disease Control and Prevention identified the nudge as a “best practice.” Other federal agencies, multiple states and the U.K. are using these techniques to improve prescribing.

Findings show that these measures are making a difference — and can accomplish even greater results as more states and regions implement the strategies.
“These interventions are low-cost and allow the prescribing clinician to retain their decision-making authority while nudging them toward better practices,” Doctor says.
Another study showed that simply regrouping how prescription options are displayed in treatment menus makes a difference. Physicians were roughly 12 percent less likely to order antibiotics unnecessarily if the options were grouped together rather than listed individually. Furthermore, Doctor and his colleagues have analyzed such factors as time of day to evaluate other influences on a prescriber’s habits.
Our studies suggest that simple and inexpensive tactics, grounded in scientific insights about human behavior, can be extremely effective in addressing public health problems.
Jason Doctor and colleagues in The New York Times
Proven Results
The effectiveness of these nudges was further demonstrated when Schaeffer Center research partners, including RAND Corp. and Northwestern University, examined what happened after the nudges were stopped. In a follow-up study published in the Journal of the American Medical Association, the team found that, 12 months after ending the peer-comparison intervention, clinicians increased their antibiotic prescription rate from 4.8 to 6.3 percent. The rate also increased from 6.1 to 10.2 percent among clinicians who were no longer asked to justify their prescriptions. These results underscore the need to adopt these interventions over the long term to ensure continued success.
